OIG to CMS: Adjust payments for orthotic devices

By HME News Staff
Updated Tue November 5, 2019
WASHINGTON - Medicare allowable amounts for certain orthotic devices are not comparable with payments made by select non-Medicare payers, according to the Office of Inspector General.
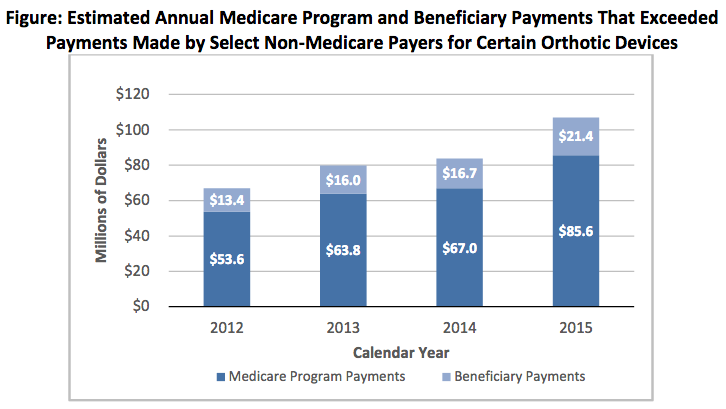
For calendar years 2012-15, the OIG estimated that Medicare and beneficiaries paid $341.7 million more than select non-Medicare payers on 142 HCPCS codes and $4.2 million less than select non-Medicare payers on 19 codes. Of the net $337.5 million difference, the agency estimated that Medicare paid $270 million and beneficiaries $67.5 million.
The reason, according to the OIG: CMS does not routinely evaluate pricing trends for orthotic devices or payments made by select non-Medicare payers; instead, it uses statutorily mandated fee schedule payments that have an economic update factor applied to them annually.
The OIG identified 95 codes for which the Medicare allowable amounts could be adjusted using existing legislative authority to make those amounts comparable with payments made by select non-Medicare payers. For the remaining 66 codes, CMS would be required to seek new legislative authority to make adjustments.
The OIG recommends that 1) CMS review the allowable amounts for the 161 codes for which Medicare and beneficiaries paid more and adjust the allowable amounts, as appropriate, using regulations promulgated under existing legislative authority or, if that's not possible, seek authority to align Medicare allowable amounts for these items; and 2) routinely review Medicare allowable amounts for new and pre-existing orthotic devices to ensure that Medicare allowable amounts are in alignment with payments made by select non-Medicare payers or pricing trends.
CMS concurred with the OIG's recommendations, saying it would consider recommending this proposal for inclusion in the president's next budget. The agency also noted that it has included a new methodology for calculating fee schedule payment amounts for new DMEPOS as part of a recent final rule.
Comments